AAACN’s Workplace Safety Task Force has recognized a significant need for enhanced tools and resources tailored to individuals working in outpatient settings, particularly concerning the issue of workplace violence. This Toolkit represents a comprehensive assembly of original, collaborative, and evidence-based materials, with a primary objective of fostering a culture of safety. It encompasses strategies for prevention, response, and support, serving as a practical manual for organizations of varying sizes to effectively address workplace violence through staff training, template development, and the provision of area-specific resources.
While workplace violence is commonly perceived as deliberate physical assault, it encompasses a spectrum of behaviors, including threats, sexual harassment, discriminatory language, and gestures. These incidents can occur across various mediums, such as in-person interactions, over the phone, via social media, or through video communication, with the interpretation of such events being deeply influenced by individual experiences.
AAACN is steadfast in its commitment to supporting ambulatory nurses in environments that prioritize both physical and psychological safety, thereby promoting overall well-being, security, and job satisfaction (AAACN, 2023). Recognizing the detrimental impact of workplace violence, incivility, and bullying on patient care quality and safety, AAACN advocates for a zero-tolerance approach. Nurses are urged to actively advocate for safe care environments, not only for themselves but also for their patients. Consequently, AAACN endeavors to equip ambulatory nurses with the necessary tools and interdisciplinary resources to uphold safety standards across all care settings.
Central to its mission, AAACN is dedicated to cultivating workplaces that are devoid of workplace violence, incivility, bullying, discrimination, and harassment. By championing this cause, the organization aims to eradicate workplace abuse and foster healthy work environments (AAACN, 2023).
The materials included in this toolkit are merely examples of materials developed and/or used by contributing health systems. These materials are made available for background informational purposes only. They are not instructions, templates, or guides for any other facility. Each facility must use its own independent judgement and experience when developing documentation/policies/procedures for its own use based on the facility’s particular circumstances, priorities, risk tolerances, and any other relevant factors.
These materials are made available on an “as-is” basis, without representation or warranty of any kind whatsoever, whether express or implied. Any use of such materials is solely at the risk of the user. By accessing or using these materials, the user acknowledges and agrees that the provider of the materials shall have no, and hereby disclaims, any responsibility or liability arising from, or related to, such access or use.
Preparation Before an Event
- Define workplace violence as an organization, and recognize all types, including face-to-face, verbal, cyber, and telephone.
- Use signage to share stance on workplace violence in your facility
- Create a Code of Conduct policy as a way to communicate the organization’s expectations to the patient and family.
- Use Code of Conduct to create plan to share policy with patients in advance of a visit via a message or phone call.
- Educate staff on workplace violence.
- (This link provides access to a free cloud-based education module by the Northwest Area Health Education Center. You will be navigating away from the AAACN website.)
- Empower nurses to handle events independently.
- Badge Buddy Example
- Create organizational-approved scripting.
- Badge Buddy Example
- Offer an overview of trauma-Informed care.
- Create awareness of how trauma-informed care impacts both patients and staff.
- Complete a security risk assessment of the care environment.
- Provide police and security training to educate staff on deescalating an event.
Before a Subsequent Event
- Develop a safety action plan.
- Implement a system for flagging patient medical records that present with safety concerns.
- Resources:
- Develop a code for violent behaviors (e.g. “Dr. Strong”).
- Implement a behavioral agreement with the patient.
- Resources:
- Consider pre-visit consultation with healthcare resources for patients with autism, SUDS (substance abuse), psychosis, and dementia.
Additional Considerations for Telephone and Cyber Incivility
Many staff feel like it is their job to “take it” when it comes to telephone verbal violence or cyber incivility.
- Educate staff that this is not acceptable behavior.
- Provide resources for staff to set appropriate boundaries with patients while engaging in communication over the phone/patient portal.
Response During an Event
- Utilize de-escalation techniques.
- Educate on possible responses to WPV events.
- Resources:
- Request immediate police and security intervention.
- Familiarize staff with possible de-escalation scripting:
- 57 Phrases to De-escalate Any Angry Customer
- Stay calm and keep a level tone of voice.
- Work through your service recovery model to determine patient’s needs and provide opportunity to rectify patient’s complaints.
- Validate patient’s feelings and set boundaries when needed.
- Encourage and allow staff to put their safety first.
During a Subsequent Event
- Request police and security standby during the visit.
- Initiate behavior agreement due to multiple events.
- Request police and security escort to staff member’s car.
Additional Considerations for Telephone and Cyber Incivility
- Develop scripting for staff to refer to during heightened telephone conversations.
- Build phrases in your charting system.
- This guides employees on how to handle difficult situations if they forget what they’ve been taught due to emotional nature of the situation
- Systemwide scripting needs to be vetted through Risk, Legal, Patient Experience, Behavioral Health, and upper leadership.
- Build phrases in your charting system.
- Use limit setting/de-escalation phrases and terminating phrases if escalation continues.
- When using a terminating call or discontinuing a message, instruct the patient to call 911 for a medical or psychiatric emergency.
Phone
- Allow staff to terminate call if boundaries are not respected.
Patient Portal
- Encourage and allow staff to step away from the message before responding.
- Re-read the sender’s message to ensure proper interpretation.
- Use patient portal-specific phrases.
- Discontinuation options:
- Determine if your charting system has the capability to stop a sender from replying further to an uncivil thread.
- Suspend patient portal communication for specific period of time.
Resources for Supporting Staff After an Event
- Huddle post-event
- Leadership to follow up with staff member to offer support.
- Connect the employee with an employee assistance program or other support systems you have in place.
- Participate in clinic-based de-briefs if needed.
- Resources:
- Schedule proactive response teams for upcoming visit.
- Escalate threats to police and security.
- Enact behavior agreement if appropriate.
- Use safety reporting system to report all workplace violence, including telephone and cyber incivility.
- Add a safety flag to the patient’s electronic medical record.
- Develop peer support related to workplace violence.
- Debrief with an external facilitator.
- Allow time for employee to decompress.
- Follow-up communication to the patient’s referring provider, if applicable.
Resources for Supporting Staff After a Subsequent Event
- Re-evaluation of plans (Safety Action Plan, Behavioral Agreement, etc)
- Update safety flag to the patient’s electronic medical record
- If behavior continues, communicate to patient that they will not be allowed to schedule appointments.
- Consider discharge or termination from practice depending on behavior, reasoning, and access to similar care
- Create a review committee
- Safety Flag reviews
- Potential discharge reviews
Additional Considerations for Telephone and Cyber Incivility
- These events may occur more often than face-to-face violence.
- Give self-care suggestions staff can use like breathing techniques, chair yoga, listening to inspirational music, and stepping away and taking a break.
References
- American Academy of Ambulatory Care Nursing [AAACN]. (2023). Scope and standards of practice for professional ambulatory care nursing(10th edition). AAACN.
- American Nurses Association. (2019). Workplace violence in nursing: Dangerous and underreported. Link
- American Nurses Association. (2015). American Nurses Association position statement on incivility, bullying, and workplace violence. ANA.
- Crisis Prevention Institute [CPI]. (2023). Top 10 de-escalation tips. Link
- Myra Golden Seminars. (2023). 57 phrases to de-escalate any angry customer. MyraGolden.com. Link
- The Joint Commission [TJC]. (2023). Information on Joint Commission standards. Link
- Mass General Brigham. (2023). Application and review of patient safety risk flags. Mass General Brigham.
- Mass General Brigham. (2023). Charter: Safety flag committee. Mass General Brigham.
- Mass General Brigham. (2023). SAFER model algorithm. Mass General Brigham.
- Novant Health. (2022). Violence toward team members, patients, or visitors is not allowed. Novant Health.
- University of Rochester Medical Center. (2021). Ambulatory services code of conduct policy. University of Rochester Medical Center.
- University of Rochester Medical Center. (2021). Code of conduct policy. University of Rochester Medical Center.
- University of Rochester Medical Center. (2023). Management of disruptive patient guidelines. University of Rochester Medical Center.
- University of Rochester Medical Center. (2022). Management of violent acts or threats of violence policy. University of Rochester Medical Center.
- University of Rochester Medical Center. (2023). MyChart message policy. University of Rochester Medical Center.
- University of Rochester Medical Center. (2022). Termination of services policy. University of Rochester Medical Center.
- University of Rochester Medical Center. (2022). The I CARE commitment. University of Rochester Medical Center.
- University of Rochester Medical Center. (2023). Working together for better health and safety. University of Rochester Medical Center.
- Vanderbilt University Medical Center. (2023). Badge buddies. Vanderbilt University Medical Center.
- Vanderbilt University Medical Center. (2023). Clinic specific safety action plan. Vanderbilt University Medical Center.
- Vanderbilt University Medical Center. (2023). Clinic specific safety action plan: Leader guide. Vanderbilt University Medical Center.
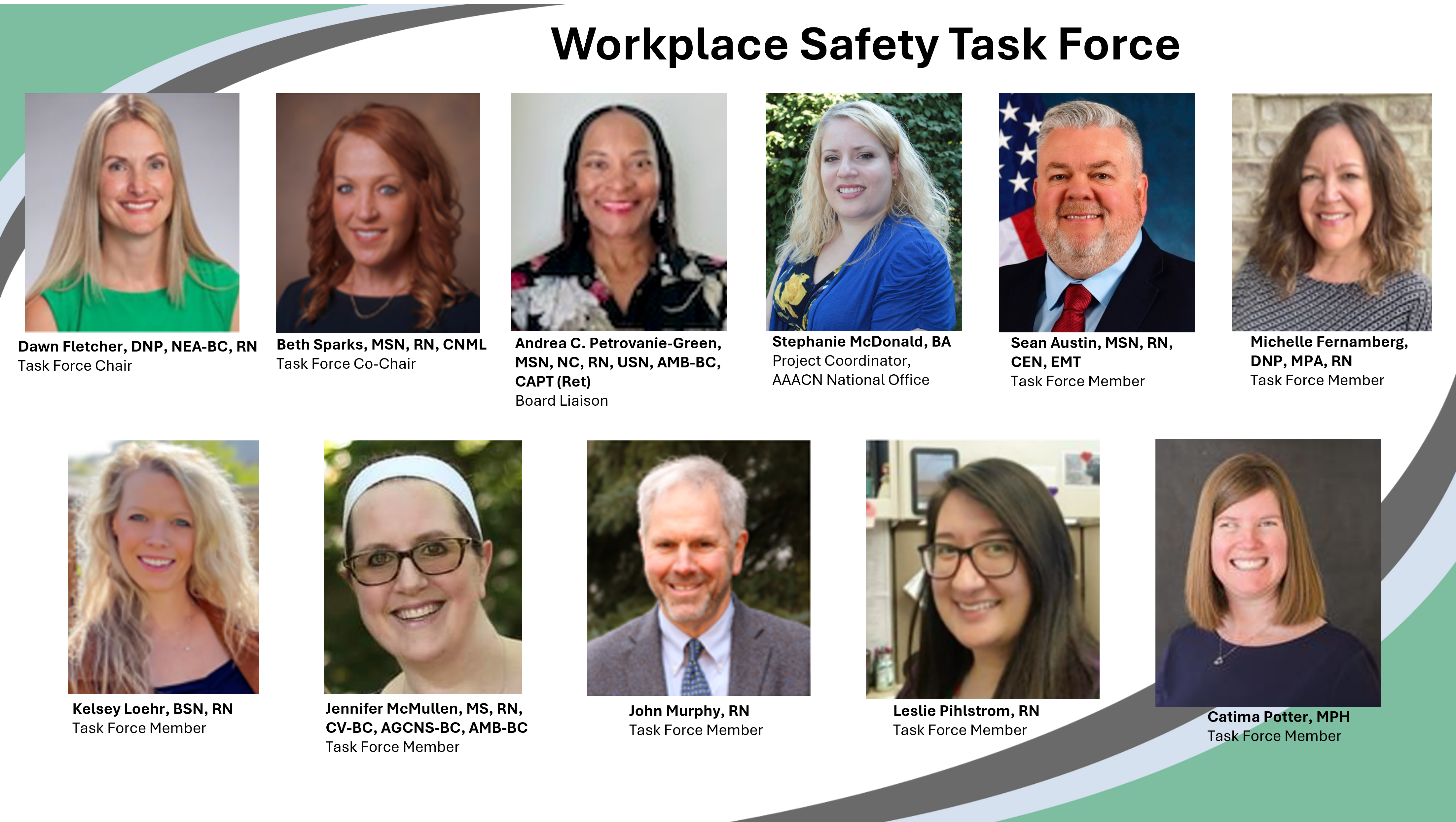
Contributors
The AAACN Board of Directors formed the Workplace Safety Task Force to develop resources to educate members on the topic of ambulatory care workplace safety and violence prevention methods. The efforts of this group are greatly appreciated.